Hugh PymHealth editor and
Kathryn Armstrong
 BBC
BBCA targeted prostate cancer screening programme for men at the highest risk could “save countless lives”, former prime minister Rishi Sunak has told the BBC.
Prostate Cancer Research, of which Sunak is a patron, has published a report on the costs and benefits of such an initiative. It would focus on black men and/or those with a family history of prostate cancer who are aged 45–69.
Sunak said he is “convinced of the urgency ” of introducing such a programme, which he believes would be affordable and deliverable.
But some medical experts are sceptical about the value of screening, arguing there is a risk patients will be treated for the cancer unnecessarily.
Prostate Cancer Research estimates the screening programme, which would involve an MRI scan, a PSA (prostate-specific antigen) blood test and a biopsy, would cost £25m a year – or about £18 per patient – similar to bowel and breast cancer screening.
It assumes 20% of eligible men – of which there are an estimated 1.3 million in the UK – would be invited annually, with a 72% uptake rate. Diagnostic activity (scans and biopsies) would need to rise by 23%, with only a modest increase in NHS staffing, the charity says.
The prostate is a walnut-shaped gland at the base of the bladder that naturally grows with age, but can sometimes become cancerous when cells grow in an uncontrolled way. Prostate cancer can be symptomless in the early stages.
Asked whether he might have done more while in Downing Street to push the case for prostate cancer screening, Sunak said testing had now become more reliable through the use of MRI scans.
“I’ve had family and friends that have been impacted by it – thankfully not lost their lives – but that partly has made me aware of why it’s so important we catch it early – the doctors are so brilliant now at treating you if you catch it early.”
Sunak said men, including himself, were often shy of coming forward to discuss health issues: “That’s why a proactive targeted screening programme could make a difference in helping save lives.”
More than 58,000 men were diagnosed with prostate cancer in England alone in 2024, a 9% increase on 2023, the latest figures from the National Prostate Cancer Audit show.
Meanwhile, one in four black men will be diagnosed with prostate cancer, compared to one in eight white men and one in 13 men of other ethnicities, according to Prostate Cancer Research. Men are also more than twice more likely to develop the cancer if they have a family history of it.
The UK National Screening Committee is currently reconsidering its decision from five years ago not to recommend routine screening. Media reports suggest it may stick with its current stance.
Urologist Prof Noel Clarke, representing the British Association of Urological Surgeons, told the national audit that while it was encouraging more men were being diagnosed and treated earlier, “we must also tackle the inequalities revealed by the audit so that age or postcode never determine the quality of care men receive”.
Oscar-winning film director Sir Steve McQueen, whose father’s own death from the disease led him to seek more information about it, agrees.
“I find it very, very difficult to think that just because people have a certain kind of privilege they can be treated. It’s unfair,” he told BBC Radio 4’s Today programme.
He added that greater prostate cancer screening could help “equalise” the situation.
Sir Steve was himself diagnosed with prostate cancer in 2022 but made a full recovery.
“I had the potential to find this cancer, my father did not. Now we have the potential to cure so many men of this, when they don’t even know they have cancer,” he said.
 PA Media
PA MediaOlympic cycling champion Sir Chris Hoy, who has advanced prostate cancer, is advocating for earlier checks.
He wants the age threshold for requesting a PSA blood test lowered. Currently, it is not routinely offered to men without symptoms who are under 50.
The PSA test is controversial, though. Levels can rise for reasons other than cancer, such as infections, leading to false positives. Critics say this can result in unnecessary treatment and side effects.
According to the report authors, the benefits of introducing targeted screening for those at the highest risk outweigh the financial and logistical costs.
Professor Hashim Ahmed, Chair of Urology at Imperial College, says more research is needed to determine the potential value of screening.
“The problem is we can often find disease that doesn’t need to be treated and we end up causing harm…and my concern at the moment is that harm to benefit equation isn’t quite right.”
Potential side effects of prostate cancer treatment are incontinence and erectile dysfunction.
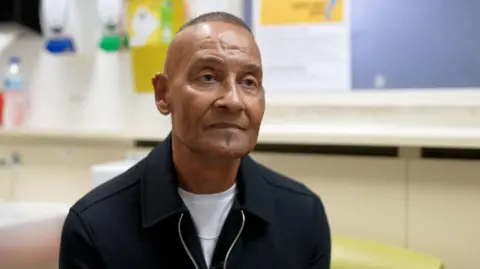
Patient voices are helping to shape the debate. On a recent visit to a prostate cancer clinic at Guy’s Hospital in London, Sunak met 66-year-old David Bateman.
He was diagnosed with the cancer at the age of 59 after asking for a SPA test, and was told it had spread to his pelvis.
Mr Bateman has since been given chemotherapy, radiotherapy and hormone treatment but cannot be cured. He supports screening for those who are potentially vulnerable.
“That is very important to me because of my sons – they are 38 and 40 – I want them checked as soon as possible. If I had been screened at 50, I am sure I wouldn’t be in the position I am today,” he said.